Enrollment and Eligibility
RSi completed its acquisition of Invicta Health Solutions at the beginning of 2023. Invicta, a Texas-based company founded in 2020, had quickly become known in the RCM marketplace for its highly competitive Enrollment and Eligibility prowess, personnel, and talent. Invicta’s reputation for progressive tech integrations, unique partnerships with established entities, and mastery of business intelligence, made it an attractive addition to the RSi portfolio. For the Invicta Enrollment leadership, becoming part of RSi has created room for service line expansion, technology development, and operational improvement.
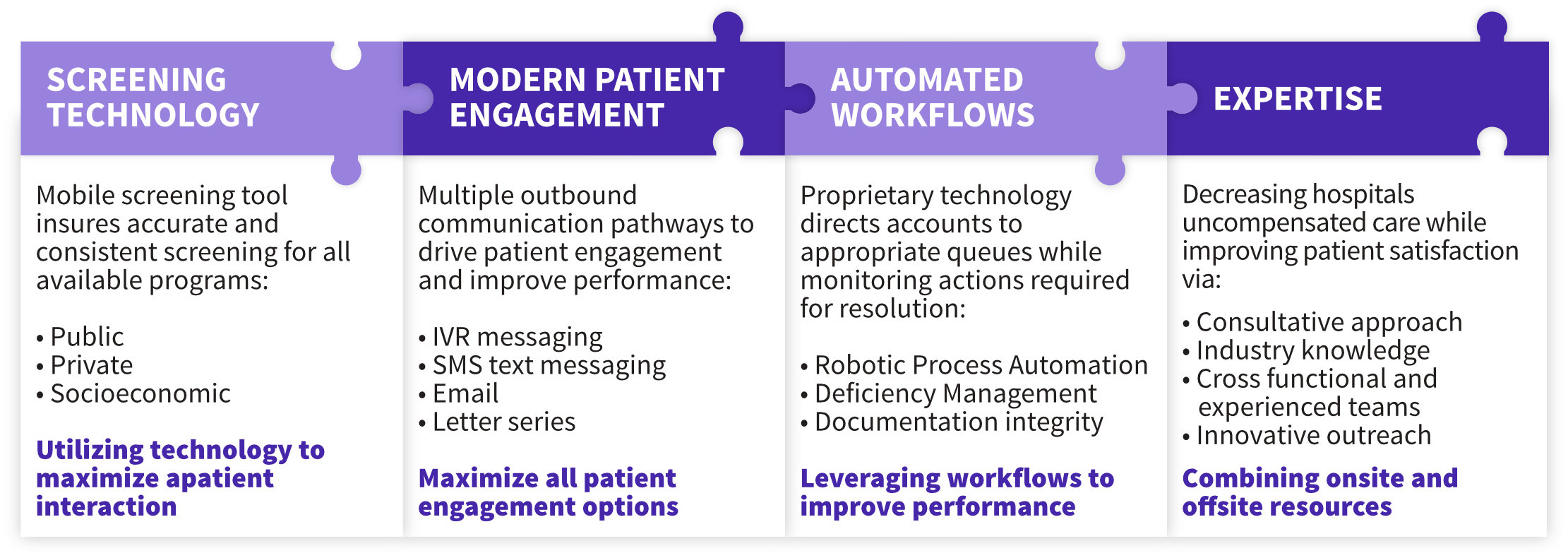
Our team leverages an ensemble of capabilities to deliver Enrollment services that positively impact the lives of patients while delivering improved financial clearance performance and reimbursement acceleration to our provider partners. Our patient-centric approach supports patients throughout the entirety of the application process, thereby elevating the patient experience and maximizing program utilization.
Enrollment Cornerstones
Technology Intellect
Our proprietary technologies support both people and process, helping us better manage data collection, enhance patient interaction, and streamline the eligibility process from program identification to application submission and approval. Modern technology enabled connectivity systems are no longer a “nice-to-have” resource: They are an absolute necessity.
Our integration of call, mail, email, IVR ,and SMS capabilities perform under a single platform that can be concurrently utilized by end users to maximize efficiency and patient response rates. Our process accelerates the workflow for our Enrollment teams tasked with primary, secondary, and outpatient enrollment. Among the most important features of the platform is its ability to accurately track individual, team, and company-wide performance and productivity in real time.




Measurement
Our Enrollment team provides unparalleled custom reporting through our in house platform and can supply reporting formats ranging from claim-level Excel files with custom data elements to comprehensive graphical dashboarding to provide executive overviews of data. Key Performance Indicators include: Number of placements; Number of Screenings; Screening Percentage of Net Referrals; Number of Applications Taken; and Conversion Rates.
Reporting
- Monthly Performance Reports
- Inpatient and Outpatient Summary Detail
- Reconciliation Reports
- Ad Hoc Reporting Available
Experienced Management
Our tenured Enrollment team is accountable for process review and best practices, technology deployment, inventory analysis, and total performance management. Our ability to hire, train, and produce high-quality team members ensures we deliver exceptional patient service and improved financial results. We recognize that we are a community support partner and strive to combine a social services approach with a strong account management system.



